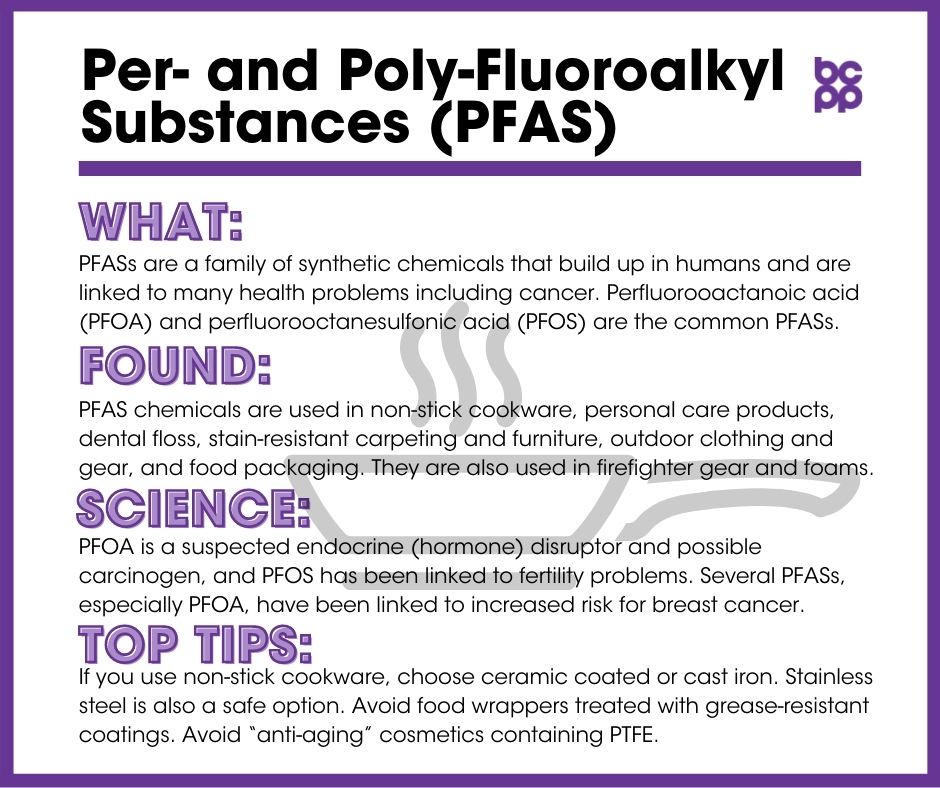
PFAS Forever Chemicals (also PFOA, PFOS)
At a Glance
Known as “Forever Chemicals,” PFAS (Per- and poly-fluoroalkyl substances) chemicals are a family of synthetic chemicals that build up in humans and are linked to numerous health problems including cancer.
The two most widely detected PFAS chemicals, perfluorooactanoic acid (PFOA) and perfluorooctanesulfonic acid (PFOS), have been used extensively in products for their properties of high stability and low surface tension. PFOA and PFOS are found in items ranging from cookware and paper food packaging to personal care products, carpeting and firefighting foam, and provide stain resistance.
PFOA is a suspected endocrine (hormone) disruptor and possible carcinogen, and PFOS has been linked to fertility problems.
Several PFAS chemicals, especially PFOA, have been linked to increased risk for breast cancer.
What are PFAS “Forever Chemicals”?
PFAS (Per- and polyfluoroalkyl substances) commonly known as “forever chemicals” are a family of chemicals that do not occur naturally in the environment. PFOA (Perfluorooctanoic Acid) and PFOS (Perfluorooctanesulfonic acid) are the most common of the PFAS family, although both are being phased out due to their adverse health and environmental effects. They are being replaced with other PFAS compounds that share their potential to repel oil, grease and water. PFASs are often called ‘forever chemicals’ as they do not break down in the environment, and are found throughout the world, in humans and other animals, as well as in our food supply.[1],[2] The most studied PFAS compounds in terms of environmental and health effects are PFOA and PFOS, followed by PFHxS and PFNA.
Although still found in almost all samples from US adults tested in the US NHANES program[3], PFAS (PFOA, PFOS, PFHxS and PFNA) levels have gone down significantly over the past 20 years.[4] PFAS chemicals are found in samples of placenta, maternal cord blood and breast milk.[5] A 2018 long term study in Finnish children demonstrated that while blood concentrations of several PFAS compounds decreased between 1-10 years of age, the full body burden increased over that period. Longer breastfeeding by infants resulted in higher blood PFAS levels when the children reached 1 year old.[6] At the same time, longer (> 6mo) duration of breastfeeding was associated with decreased levels of PFAS in the mothers’ blood.[7] These findings are consistent with the observation that PFASs are found in breast milk and passed on to the infant during breastfeeding.[8] A 2020 study from China found a lower infant growth rate with higher exposure to PFASs during breastfeeding.[9] Breastfeeding is still the best option for newborn and infant nutrition.
Exposures to several PFAS chemicals—including PFOS, PFHxS, PFNA, PFDA and PFHpS—are associated with earlier onset of several markers of puberty in girls. Many of these relationships are non-linear, that is, effects on puberty were more marked at the middle levels of PFAS concentration than at either the high or low ends.[10]
Due to these and other health concerns, and nascent international legal restrictions, PFOA and PFOS have been voluntarily phased out of use. Because of their persistence, they are still found in wildlife across the planet.[11],[12] This has led manufacturers to begin replacing the longer-chain PFAS chemicals such as PFOA and PFOS with shorter-chain acids. These newer chemicals may be less toxic and bioaccumulative (builds up less in humans and other organisms), although emerging data indicate that many shorter-chain PFAS chemicals may also have negative health effects.[13]
PFOA (Perfluorooactanoic acid)
PFOA (Perfluorooactanoic acid) is a highly fluorinated compound with low surface tension, making it an effective chemical to help make products non-stick, water resistant and stain resistant. PFOA has been used to make PTFE (polytetrafluoroethylene), and can be found at contaminant levels in products containing PTFE, such as Gore-Tex®, Teflon® and anti-aging cosmetics. A 2019 study has also found PFOA in dental floss materials.[14] Another found higher levels of PFOA, and other PFAS compounds, in blood samples after people ate at fast food restaurants, or consumed either pizza or microwave popcorn at home.[15] Because PFOA is persistent in the environment (it does not break down), it is a common contaminant in drinking water.[16] PFOA is also found in indoor dust, especially in newly renovated buildings or homes with new upholstered furniture or carpeting.[17],[18] PFOA is very stable and bioaccumulates in the blood and in tissues such as lung and kidney in people and animals.[19],[20] Increased intake of PFOA through breastfeeding decreased the diversity of infants’ gut microbiome,[21] a factor that has been associated with increased risk for developing breast cancer in adults.[22] Higher exposure to PFOA in early childhood was associated with decreased Body Mass Index, HDL-cholesterol levels (thought of as “bad” cholesterol) and borderline insulin resistance in 6-8 year old girls.[23]
Both the International Agency for Research on Cancer (IARC) and the U.S. Environmental Protection Agency (EPA) have designated PFOA a potential human carcinogen.[24] In addition, there have been several findings that exposure to PFOA could be associated with endocrine (hormone) disruption and an increased risk of developing breast cancer (see below).
PFOS (Perfluorooctanesulfonic acid)
PFOS (Perfluorooctanesulfonic acid) is closely related to PFOA, and is also ubiquitous in the environment. Its main use has been as a stain repellant and fabric protector; it is the main ingredient in Scotchguard® and is also an ingredient in firefighting foam. PFOS levels in the US population have been decreasing over the past decade as the chemical has been phased out of use in the United States.[25] Still, PFOS is found ubiquitously in human samples and has been detected in amniotic fluid[26] and umbilical cord blood,[27] and is associated with lower weights at birth but higher weights at 20 months of age.[28]
PFOSA (Perfluorooctane sulfonamide) is a PFAS compound that breaks down to PFOS in the environment. It has been found to damage the health of cells and their ability to process fats in salmon liver cells.[29]
PFHxS (Perfluorohexane sulfonic acid)
PFHxS (Perfluorohexane sulfonic acid) is also ubiquitous in the environment. One study detected PFHxS in nearly all people tested for PFASs.[30] An analysis of water and fish contaminated by an accidental release of firefighting foam in Canada found a small amount of PFHxS present.[31] A Swedish study detected high levels of several PFASs including PFHxS in firefighters compared to a control group[32] and a 2020 study found that female San Francisco firefighters, as compared to office workers, had more than twice the levels of serum PFHxS (along with raised levels of PFUnDA and PFNA).[33]
PFHxS has been found to alter development, especially in the reproductive system, in rats.[34] PFHxS along with other PFASs have been detected in breast milk, and it was concluded that breastfeeding is a considerable source of exposure to perfluorinated chemicals for infants.[35] Despite these findings, breastfeeding remains the best option for newborn and infant nutrition.
PFNA (Perfluorononanoic acid) and PFDoA (Perfluorododecanoic acid)
PFNA (Perfluorononanoic acid) and PFDoA (Perfluorododecanoic acid) are synthetic perfluorinated chemicals that have been found in humans and wildlife worldwide. PFNA may lead to developmental and reproductive toxicity to males.[36],[37] Several epidemiological studies have found a link between PFOS, PFOA and PFNA and reduced semen quality.[38],[39],[40] PFDoA has been found to affect the reproductive function of male rats.[41]
PFOA & PFOS substitutes
Perfluorohexanoic acid (PFHxA) and Perfluoroheptanoic acid (PFHpA) are shorter chain PFASs that have been detected in drinking water.[42] Some researchers believe that the increasing content of short chain PFASs in water reflects increased use of these PFASs as replacements for PFOS and PFOA-related substances.[43] Early research suggests PFHxA and PFHpA may be developmental toxicants. PFHpA demonstrated more severe effects on liver and heart development than PFHxA.[44]
Perfluorobutane sulfonic acid (PFBS) was developed in 2003 as a PFOS replacement. PFBS has been found in drinking water and samples of whole fish including striped mullet, anchovies, young hake and swordfish fillets.[45] Since 2003, it has also been marketed as a stain resistant treatment for carpets.[46] One study found PFBS in household cleaning products between 2007 and 2011.[47] It has been suggested that PFBS could affect neuronal development[48] and potentially alter the hormonal system by allowing imbalances between androgens and estrogens.[49],[50]
Perfluorooctane sulfonamide (PFOSA) has been found to damage the health of cells and their ability to process fats in salmon liver cells.[51] In people, higher PFOSA levels have been associated with changes in kidney function.[52]
Perfluorobutyric acid (PFBA) is part of the perfluoroalkyl family and low levels have been detected in drinking water.[53] A 2014 study found high accumulation levels on lettuce and strawberries irrigated with reclaimed water.[54] PFBA has also been found in donor blood serum samples[55] and in samples from ski wax technicians who were exposed to high levels of PFASs.[56]
Where are PFAS chemicals found?
PFAS chemicals can be found in non-stick cookware, personal care products, dental floss, stain-resistant carpeting and furniture, outdoor clothing and gear, and food packaging and contact paper (e.g., fast food wrappers, microwave popcorn bags). PFAS are also found in firefighter turnout gear (personal protective gear) and foams. [57]
What evidence links PFAS “Forever Chemicals” to breast cancer?
- A study of Inuit women in Greenland showed that women with higher blood serum levels of PFOS, PFOA and total PFAS have an increased risk of breast cancer.[58] In a more recent follow-up of this cohort, higher total serum PFASs, as well as levels of PFOA, PFOS, PFHxS were associated with increased risk for developing breast cancer.[59]
- A study on pregnant Danish women and serum levels of PFAS found a significant positive association with PFOSA and breast cancer.[60]
- A French study found no overall association between serum PFAS levels and risk of breast cancer. There was a significant positive association between PFOS levels and ER+ breast cancer, but only in the second quartile of PFOS concentrations. Similarly, the second quartile (and not higher or lower) concentrations of PFOA was associated with increased risk of ER- breast cancer. These results support the notion that many endocrine disrupting compounds exert their negative health effects through nonlinear processes.[61]
- A study embedded within the California Teacher’s study found no overall association between total PFAS levels at 15 months after diagnosis and risk of developing breast cancer, as compared with age-matched controls. However, there was an association with higher PFHxS levels and the risk of hormone receptor negative (ER-/PR-) breast cancer.[62]
- Recent studies are beginning to look at modifying factors that may influence whether associations exist between PFAS levels and risk of breast cancer. A 2019 report from the Child Health and Development Studies cohort looked at PFAS and cholesterol levels in maternal blood around the time of giving birth and risk of their daughters developing breast cancer before the age of 52 years. Higher maternal PFOS levels were associated with a decreased risk of their daughters developing breast cancer. However, higher maternal levels of a precursor to PFOS, in combination with higher levels of maternal cholesterol, were associated with a 3.6-fold increase in their daughters’ breast cancer risk. Higher cholesterol levels have been independently associated with increased risk for developing breast cancer, possibly through its effects on estrogen-stimulating pathways.[63]
- A 2017 Danish study has shown that women who have a variability in the structures of the genes involved in the synthesis and metabolism of estradiol may be more sensitive to the effects of PFOSA (a precursor of PFOS) on increased risk for breast cancer.[64]
- Higher levels of PFOA and PFOS are associated with difficulty conceiving, longer delays in becoming pregnant[65] and early onset of menopause in women.[66],[67]
- Studies in rodents have shown that exposure to PFOA can delay development of mammary glands, reduce birthweight and cause neonatal death.[68],[69],[70]
- Exposure to PFOA can disrupt lactation in mothers and alter development of mammary glands in female mouse pups.[71]
- Cell culture studies examine possible mechanisms by which compounds including PFASs might alter risk for developing breast cancer. One study found that both PFOA and PFOS enhanced the effects of estradiol in hormone-dependent human breast cancer cells.[72] Another found that PFOA increased the rate of cell proliferation and neoplastic activity of normal (non-tumor) human epithelial cells.[73]
Who is most likely to be exposed to PFAS “Forever Chemicals”?
PFAS chemicals are ubiquitous,[74] meaning that almost everyone will be exposed to at least small amounts.[75] People living near PFOA manufacturing sites, contaminated military sites and regions with PFOA-impacted drinking water may be at risk for exposure to higher levels of PFOA.[76] Firefighters, especially officers and those actively fighting fires (as compared with drivers) are exposed to significant levels of PFASs.[77]
Who is most vulnerable to the health effects of PFAS “Forever Chemicals”?
Women, particularly pregnant women, and children are most vulnerable to the potential health effects of PFAS chemical exposure.
What are the top tips to avoid exposure to PFAS “Forever Chemicals”?
- Do not use non-stick cookware made from per- and poly-fluorinated substances. Instead, use ceramic coated non-stick or well-seasoned cast iron cookware.
- Avoid food contact paper treated with grease-resistant coatings, like paper wrapping and coated cardboard boxes used at fast food restaurants.
- Avoid “anti-aging” cosmetics containing PTFE.
- People living in areas with PFOA contaminated drinking water should consider drinking bottled water.
Additional Resources
Madrid Statement (Scientific Consensus Statement) May 2015
Zurich Statement on Future Actions on PFASs
[2] Xiao, Feng. “Emerging poly- and perfluoroalkyl substances in the aquatic environment: A review of current literature.” Water Research 124 (2017): 482-495. doi:10.1016/j.watres.2017.07.024.
[3] Centers for Disease Control and Prevention. “National Report on Human Exposure to Environmental Chemicals.” Last modified April 14, 2017. https://www.cdc.gov/exposurereport/.
[4] Agency for Toxic Substances and Disease Registry. “Perfluoroalkyl and Polyfluoroalkyl Substances (PFAS) in the U.S. Population.” Last modified August 21, 2017. https://www.atsdr.cdc.gov/pfas/docs/PFAS_in_People.pdf.
[5] Müller, M H B et al. “Prenatal exposure to persistent organic pollutants in Northern Tanzania and their distribution between breast milk, maternal blood, placenta and cord blood.” Environmental Research 170 (2019): 433-442. doi:10.1016/j.envres.2018.12.026.
[6] Koponen, Jani et al. “Longitudinal trends of per- and polyfluoroalkyl substances in children’s serum.” Environment International 121, 1 (2018): 591-599. doi:10.1016/j.envint.2018.09.006.
[7] Colles, Ann et al. “Perfluorinated substances in the Flemish population (Belgium): Levels and determinants of variability in exposure.” Chemosphere 242 (2020): 125250. doi:10.1016/j.chemosphere.2019.125250.
[8] Abdallah MA, et al. “Concentrations of perfluoroalkyl substances in human milk from Ireland: Implications for adult and nursing infant exposure.” Chemosphere 246 (2020):125724. doi:10.1016/j.chemosphere.2019.125724.
[9] Jin, Hangbiao et al. “Poly- and perfluoroalkyl substance concentrations in human breast milk and their associations with postnatal infant growth.” The Science of the Total Environment 713 (2020): 136417. doi:10.1016/j.scitotenv.2019.136417.
[10] Ernst, Andreas et al. “Exposure to Perfluoroalkyl Substances during Fetal Life and Pubertal Development in Boys and Girls from the Danish National Birth Cohort.” Environmental Health Perspectives 127, 1 (2019): 17004. doi:10.1289/EHP3567.
[11] Jensen, Allan Astrup, and Henrik Leffers. “Emerging endocrine disrupters: perfluoroalkylated substances.” International Journal of Andrology 31, 2 (2008): 161-9. doi:10.1111/j.1365-2605.2008.00870.x.
[12] Kato, Kayoko et al. “Trends in exposure to polyfluoroalkyl chemicals in the U.S. Population: 1999-2008.” Environmental Science & Technology 45, 19 (2011): 8037-45. doi:10.1021/es1043613.
[13] Pelch, Katherine E et al. “PFAS health effects database: Protocol for a systematic evidence map.” Environment International 130 (2019): 104851. doi:10.1016/j.envint.2019.05.045.
[14] Boronow, Katherine E et al. “Serum concentrations of PFASs and exposure-related behaviors in African American and non-Hispanic white women.” Journal of Exposure Science & Environmental Epidemiology 29, 2 (2019): 206-217. doi:10.1038/s41370-018-0109-y.
[15] Susmann, Herbert P et al. “Dietary Habits Related to Food Packaging and Population Exposure to PFASs.” Environmental Health Perspectives 127,10 (2019): 107003. doi:10.1289/EHP4092.
[16] United States Environmental Protection Agency. “Drinking Water Health Advisories for PFOA and PFOS.” Last modified October 16, 2020. https://www.epa.gov/ground-water-and-drinking-water/drinking-water-health-advisories-pfoa-and-pfos.
[17] Fraser, Alicia J et al. “Polyfluorinated compounds in serum linked to indoor air in office environments.” Environmental Science & Technology 46, 2 (2012): 1209-15. doi:10.1021/es2038257.
[18] Zhang, Tao et al. “Perfluorochemicals in meat, eggs and indoor dust in China: assessment of sources and pathways of human exposure to perfluorochemicals.” Environmental Science & Technology 44, 9 (2010): 3572-9. doi:10.1021/es1000159.
[19] Pérez, Francisca et al. “Accumulation of perfluoroalkyl substances in human tissues.” Environment International 59 (2013): 354-62. doi:10.1016/j.envint.2013.06.004.
[20] European Chemicals Agency. “Member State Committee Support Document for Identification of Pentadecafluorooctanoic Acid (PFOA), as a substance of very high concern because of its CMR and PBT properties.” Last modified June 14, 2013. http://echa.europa.eu/documents/10162/8059e342-1092-410f-bd85-80118a5526f5.
[21] Iszatt, Nina et al. “Environmental toxicants in breast milk of Norwegian mothers and gut bacteria composition and metabolites in their infants at 1 month.” Microbiome 7, 1 (2019): 34. doi:10.1186/s40168-019-0645-2.
[22] Parida, Sheetal, and Dipali Sharma. “The Microbiome-Estrogen Connection and Breast Cancer Risk.” Cells 8, 12 (2019): 1642. doi:10.3390/cells8121642.
[23] Fassler, Cecily S et al. “Complex relationships between perfluorooctanoate, body mass index, insulin resistance and serum lipids in young girls.” Environmental Research 176 (2019): 108558. doi:10.1016/j.envres.2019.108558.
[24] United States Environmental Protection Agency. “Technical Fact Sheet: Perfluorooctonate Sulfate (PFOS) and Perfluorooctanic Acid (PFAS).” Last modified November 2017. https://www.epa.gov/sites/production/files/2017-12/documents/ffrrofactsheet_contaminants_pfos_pfoa_11-20-17_508_0.pdf.
[25] Kato, Kayoko et al. “Trends in exposure to polyfluoroalkyl chemicals in the U.S. Population: 1999-2008.” Environmental Science & Technology 45, 19 (2011): 8037-45. doi:10.1021/es1043613.
[26] Stein, Cheryl R et al. “Comparison of polyfluoroalkyl compound concentrations in maternal serum and amniotic fluid: a pilot study.” Reproductive Toxicology 34, 3 (2012): 312-6. doi:10.1016/j.reprotox.2012.05.039.
[27] Apelberg, Benjamin J et al. “Determinants of fetal exposure to polyfluoroalkyl compounds in Baltimore, Maryland.” Environmental Science & Technology 41, 11 (2007): 3891-7. doi:10.1021/es0700911.
[28] Maisonet, Mildred et al. “Maternal concentrations of polyfluoroalkyl compounds during pregnancy and fetal and postnatal growth in British girls.” Environmental Health Perspectives 120, 10 (2012): 1432-7. doi:10.1289/ehp.1003096.
[29] Wågbø AM et al. “Perfluorooctane sulfonamide-mediated modulation of hepatocellular lipid homeostasis and oxidative stress responses in Atlantic salmon hepatocytes.” Chemical Research in Toxicology 25, 6(2012): 1253-1264. doi:10.1021/tx300110u.
[30] Calafat, Antonia M et al. “Polyfluoroalkyl chemicals in the U.S. population: data from the National Health and Nutrition Examination Survey (NHANES) 2003-2004 and comparisons with NHANES 1999-2000.” Environmental Health Perspectives 115, 11 (2007): 1596-602. doi:10.1289/ehp.10598.
[31] Moody, Cheryl A et al. “Monitoring perfluorinated surfactants in biota and surface water samples following an accidental release of fire-fighting foam into Etobicoke Creek.” Environmental Science & Technology 36, 4 (2002): 545-51. doi:10.1021/es011001+.
[32] Rotander, Anna et al. “Novel fluorinated surfactants tentatively identified in firefighters using liquid chromatography quadrupole time-of-flight tandem mass spectrometry and a case-control approach.” Environmental Science & Technology 49, 4 (2015): 2434-42. doi:10.1021/es503653n.
[33] Trowbridge, Jessica et al. “Exposure to Perfluoroalkyl Substances in a Cohort of Women Firefighters and Office Workers in San Francisco.” Environmental Science & Technology 54, 6 (2020): 3363-3374. doi:10.1021/acs.est.9b05490.
[34] Ramhøj, Louise et al. “Perfluorohexane Sulfonate (PFHxS) and a Mixture of Endocrine Disrupters Reduce Thyroxine Levels and Cause Antiandrogenic Effects in Rats.” Toxicological Sciences 163, 2 (2018): 579-591. doi:10.1093/toxsci/kfy055.
[35] Kärrman, Anna et al. “Exposure of perfluorinated chemicals through lactation: levels of matched human milk and serum and a temporal trend, 1996-2004, in Sweden.” Environmental Health Perspectives 115, 2 (2007): 226-30. doi:10.1289/ehp.9491.
[36] Feng, Yixing et al. “Effects of PFNA exposure on expression of junction-associated molecules and secretory function in rat Sertoli cells.” Reproductive Toxicology 30, 3 (2010): 429-37. doi:10.1016/j.reprotox.2010.05.010.
[37] Das, Kaberi P et al. “Developmental toxicity of perfluorononanoic acid in mice.” Reproductive Toxicology 51 (2015): 133-44. doi:10.1016/j.reprotox.2014.12.012.
[38] Joensen, Ulla Nordström et al. “Do perfluoroalkyl compounds impair human semen quality?.” Environmental Health Perspectives 117, 6 (2009): 923-7. doi:10.1289/ehp.0800517.
[39] Toft, G et al. “Exposure to perfluorinated compounds and human semen quality in Arctic and European populations.” Human Reproduction 27, 8 (2012): 2532-40. doi:10.1093/humrep/des185.
[40] Louis, Germaine M Buck et al. “Perfluorochemicals and human semen quality: the LIFE study.” Environmental Health Perspectives 123, 1 (2015): 57-63. doi:10.1289/ehp.1307621.
[41] Shi, Zhimin et al. “Alterations in gene expression and testosterone synthesis in the testes of male rats exposed to perfluorododecanoic acid.” Toxicological Sciences 98, 1 (2007): 206-15. doi:10.1093/toxsci/kfm070.
[42] Biomonitoring California. “Potential Designated Chemicals: Perfluoroalkyl and polyfluoroalkyl substances.” Last modified March 3, 2015. https://biomonitoring.ca.gov/sites/default/files/downloads/PotenDesigPFASs_031315.pdf.
[43] Rahman, Mohammad Feisal et al. “Behaviour and fate of perfluoroalkyl and polyfluoroalkyl substances (PFASs) in drinking water treatment: a review.” Water Research 50 (2014): 318-40. doi:10.1016/j.watres.2013.10.045.
[44] Kim, Miran et al. “Perfluoroheptanoic acid affects amphibian embryogenesis by inducing the phosphorylation of ERK and JNK.” International Journal of Molecular Medicine 36, 6 (2015): 1693-700. doi:10.3892/ijmm.2015.2370.
[45] Wang, Yuan et al. “Identification, Tissue Distribution, and Bioaccumulation Potential of Cyclic Perfluorinated Sulfonic Acids Isomers in an Airport Impacted Ecosystem.” Environmental Science & Technology 50, 20 (2016): 10923-10932. doi:10.1021/acs.est.6b01980.
[46] Biomonitoring California. “Potential Designated Chemicals: Perfluoroalkyl and polyfluoroalkyl substances.” Last modified March 3, 2015. https://biomonitoring.ca.gov/sites/default/files/downloads/PotenDesigPFASs_031315.pdf.
[47] Liu, Xiaoyu et al. “Concentrations and trends of perfluorinated chemicals in potential indoor sources from 2007 through 2011 in the US.” Chemosphere 98 (2014): 51-7. doi:10.1016/j.chemosphere.2013.10.001.
[48] Slotkin, Theodore A et al. “Developmental neurotoxicity of perfluorinated chemicals modeled in vitro.” Environmental Health Perspectives 116, 6 (2008): 716-22. doi:10.1289/ehp.11253.
[49] Gorrochategui, Eva et al. “Perfluorinated chemicals: differential toxicity, inhibition of aromatase activity and alteration of cellular lipids in human placental cells.” Toxicology and Applied Pharmacology 277, 2 (2014): 124-30. doi:10.1016/j.taap.2014.03.012.
[50] Biomonitoring California. “Potential Designated Chemicals: Perfluoroalkyl and polyfluoroalkyl substances.” Last modified March 3, 2015. https://biomonitoring.ca.gov/sites/default/files/downloads/PotenDesigPFASs_031315.pdf.
[51] Wågbø AM et al. “Perfluorooctane sulfonamide-mediated modulation of hepatocellular lipid homeostasis and oxidative stress responses in Atlantic salmon hepatocytes.” Chemical Research in Toxicology 25, 6 (2012): 1253-1264. doi:10.1021/tx300110u.
[52] Blake, Bevin E et al. “Associations between longitudinal serum perfluoroalkyl substance (PFAS) levels and measures of thyroid hormone, kidney function, and body mass index in the Fernald Community Cohort.” Environmental Pollution 242, A (2018): 894-904. doi:10.1016/j.envpol.2018.07.042.
[53] Rahman, Mohammad Feisal et al. “Behaviour and fate of perfluoroalkyl and polyfluoroalkyl substances (PFASs) in drinking water treatment: a review.” Water Research 50 (2014): 318-40. doi:10.1016/j.watres.2013.10.045.
[54] Blaine, Andrea C, et al. “Perfluoroalkyl Acid Uptake In Lettuce (lactuca Sativa) and Strawberry (fragaria Ananassa) Irrigated with Reclaimed Water.” Environmental Science & Technology 48, 24 (2014): 14361-14368. doi:10.1021/es504150h.
[55] Lee, Holly, and Scott A Mabury. “A pilot survey of legacy and current commercial fluorinated chemicals in human sera from United States donors in 2009.” Environmental Science & Technology 45, 19 (2011): 8067-74. doi:10.1021/es200167q.
[56] Nilsson, Helena et al. “Biotransformation of fluorotelomer compound to perfluorocarboxylates in humans.” Environment International 51 (2013): 8-12. doi:10.1016/j.envint.2012.09.001.
[57] Trowbridge, Jessica et al. “Exposure to Perfluoroalkyl Substances in a Cohort of Women Firefighters and Office Workers in San Francisco.” Environmental Science & Technology 54, 6 (2020): 3363-3374. doi:10.1021/acs.est.9b05490.
[58] Bonefeld-Jorgensen, Eva C et al. “Perfluorinated compounds are related to breast cancer risk in Greenlandic Inuit: a case control study.” Environmental Health 10 (2011): 88. doi:10.1186/1476-069X-10-88.
[59] Wielsøe, Maria et al. “Serum levels of environmental pollutants is a risk factor for breast cancer in Inuit: a case control study.” Environmental Health 16,1 (2017): 56. doi:10.1186/s12940-017-0269-6.
[60] Bonefeld-Jørgensen, Eva C et al. “Breast cancer risk after exposure to perfluorinated compounds in Danish women: a case-control study nested in the Danish National Birth Cohort.” Cancer Causes & Control 25, 11 (2014): 1439-48. doi:10.1007/s10552-014-0446-7.
[61] Mancini, Francesca Romana et al. “Perfluorinated alkylated substances serum concentration and breast cancer risk: Evidence from a nested case-control study in the French E3N cohort.” International Journal of Cancer 146, 4 (2020): 917-928. doi:10.1002/ijc.32357.
[62] Hurley, Susan et al. “Breast cancer risk and serum levels of per- and poly-fluoroalkyl substances: a case-control study nested in the California Teachers Study.” Environmental Health 17, 1 (2018): 83. doi:10.1186/s12940-018-0426-6.
[63] Cohn, Barbara A. et al. “In utero exposure to poly− and perfluoroalkyl substances (PFASs) and subsequent breast cancer.” Reproductive Toxicology 92 (2020): 112-119. doi:10.1016/j.reprotox.2019.06.012.
[64] Ghisari, Mandana et al. “Polymorphism in xenobiotic and estrogen metabolizing genes, exposure to perfluorinated compounds and subsequent breast cancer risk: A nested case-control study in the Danish National Birth Cohort.” Environmental Research 154 (2017): 325-333. doi:10.1016/j.envres.2017.01.020.
[65] Fei, Chunyuan et al. “Maternal levels of perfluorinated chemicals and subfecundity.” Human Reproduction 24, 5 (2009): 1200-5. doi:10.1093/humrep/den490.
[66] Knox, Sarah S et al. “Implications of early menopause in women exposed to perfluorocarbons.” The Journal of Clinical Endocrinology and Metabolism 96, 6 (2011): 1747-53. doi:10.1210/jc.2010-2401.
[67] Fei, Chunyuan et al. “Fetal growth indicators and perfluorinated chemicals: a study in the Danish National Birth Cohort.” American Journal of Epidemiology 168, 1 (2008): 66-72. doi:10.1093/aje/kwn095.
[68] White, Sally S et al. “Gestational and chronic low-dose PFOA exposures and mammary gland growth and differentiation in three generations of CD-1 mice.” Environmental Health Perspectives 119, 8 (2011): 1070-6. doi:10.1289/ehp.1002741.
[69] Lau, Christopher et al. “Perfluoroalkyl acids: a review of monitoring and toxicological findings.” Toxicological Sciences 99, 2 (2007): 366-94. doi:10.1093/toxsci/kfm128.
[70] United States Environmental Protection Agency. “Technical Fact Sheet: Perfluorooctonate Sulfate (PFOS) and Perfluorooctanic Acid (PFAS).” Last modified November 2017. https://www.epa.gov/sites/production/files/2017-12/documents/ffrrofactsheet_contaminants_pfos_pfoa_11-20-17_508_0.pdf.
[71] White, Sally S et al. “Gestational PFOA exposure of mice is associated with altered mammary gland development in dams and female offspring.” Toxicological Sciences96,1 (2007): 133-44. doi:10.1093/toxsci/kfl177.
[72] Sonthithai, Pacharapan et al. “Perfluorinated chemicals, PFOS and PFOA, enhance the estrogenic effects of 17β-estradiol in T47D human breast cancer cells.” Journal of Applied Toxicology 36, 6 (2016): 790-801. doi:10.1002/jat.3210.
[73] Pierozan, Paula et al. “Perfluorooctanoic acid (PFOA) exposure promotes proliferation, migration and invasion potential in human breast epithelial cells.” Archives of Toxicology 92,5 (2018): 1729-1739. doi:10.1007/s00204-018-2181-4.
[74] Jensen, Allan Astrup, and Henrik Leffers. “Emerging endocrine disrupters: perfluoroalkylated substances.” International Journal of Andrology 31, 2 (2008): 161-9. doi:10.1111/j.1365-2605.2008.00870.x.
[75] Calafat, Antonia M et al. “Exposure of the U.S. population to bisphenol A and 4-tertiary-octylphenol: 2003-2004.” Environmental Health Perspectives 116, 1 (2008): 39-44. doi:10.1289/ehp.10753.
[76] Sunderland, Elsie M et al. “A review of the pathways of human exposure to poly- and perfluoroalkyl substances (PFASs) and present understanding of health effects.” Journal of Exposure Science & Environmental Epidemiology 29, 2 (2019): 131-147. doi:10.1038/s41370-018-0094-1.
[77] Trowbridge, Jessica et al. “Exposure to Perfluoroalkyl Substances in a Cohort of Women Firefighters and Office Workers in San Francisco.” Environmental Science & Technology 54, 6 (2020): 3363-3374. doi:10.1021/acs.est.9b05490.