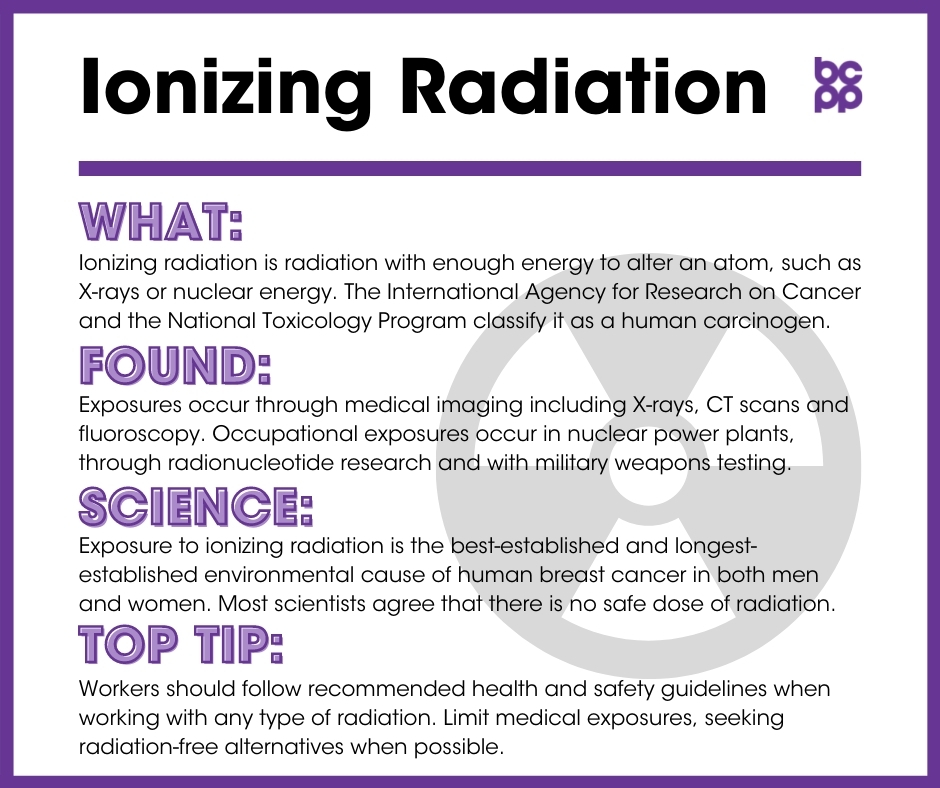
Ionizing Radiation
At a Glance
Ionizing radiation is any form of radiation with enough energy to alter an atom, such as X-rays or nuclear energy. Evidence from studies of medical exposures to radiation as well as large-scale disasters such as exposures from the atomic bomb in Japan has demonstrated that radiation can cause breast cancer.
The International Agency for Research on Cancer (IARC) and the National Toxicology Program (NTP) classify it as a known human carcinogen.
What is ionizing radiation?
Ionizing radiation is any form of radiation with enough energy to break off electrons from atoms (meaning to ionize the atoms). This radiation can break the chemical bonds in molecules, including DNA molecules, thereby disturbing their normal functioning. X-rays and gamma rays are the only major forms of radiation with sufficient energy to penetrate and damage body tissue below the surface of the skin.
Where is ionizing radiation found?
Ionizing radiation exposures occur in a variety of medical and occupational settings as well as from disasters such as the dropping of the atomic bomb in Japan.
- Medical radiological procedures:
- X-rays
- Computed tomography (CT) scans
- Fluoroscopy, a medical diagnostic test that shows moving parts, often used in cardiovascular procedures
- Sources of gamma ray emissions:
- Nuclear power plants
- Radionucleotide research
- Military weapons testing
- Nuclear medicine procedures such as bone, thyroid and lung scans
- Prior to 2013, backscatter X-ray screening machines led to exposures in airports.
What evidence links ionizing radiation to breast cancer?
Exposure to ionizing radiation is the best-established and longest-established environmental cause of human breast cancer in both men and women. Most scientists agree that no safe dose of radiation has been identified.[1],[2] Repeated low-dose exposures over time may have the same harmful effects as a single high-dose exposure.
- The link between radiation exposure and breast cancer has been demonstrated in survivors of the atomic bombing in Japan, particularly among women who were younger than 20 when the bombs were dropped.[3],[4],[5],[6], The effect of radiation exposure was especially strong for women whose age of menarche was 12 or younger and who were exposed by age 20.[7]
- Ionizing radiation can increase the risk for breast cancer by a number of different mechanisms, including direct mutagenesis, genome instability[8],[9] and changes in breast cell micro-environments that can lead to damaged regulation of cell-cell interactions within the breast.[10],[11],[12]
- Ionizing radiation not only affects cells that are directly exposed, but can alter the DNA, cell growth and cell-cell interactions of neighboring cells, a phenomenon referred to as the “bystander effect.”[13]
- While exposures to ionizing radiation from radon gas are not associated with and overall increased risk for breast cancer, there is a specific association of exposure to radon and increased risk for PR-/ER- breast cancers.
- Ionizing radiation not only affects cells that are directly exposed, but can alter the DNA, cell growth and cell-cell interactions of neighboring cells, a phenomenon referred to as the “bystander effect.”[14],[15]
Occupational exposures
- Studies show increased risk of breast cancer among radiological technologists who began working during their teens or were working in the field before the 1940s.[16], [17]
- It was also found that technologists who began working before 1950 and had worked for at least five years had an increased mortality rate from breast cancer.[18] Levels of exposure before 1950 were much higher than those found for technologists today.
- A review and analysis of all existing related studies found that women who work as airline flight attendants were exposed to higher cosmic radiation while flying and also had increased levels of breast cancer.[19]
Medical radiation
Although there has been a substantial decrease in exposures to ionizing radiation from individual X-rays over the past several decades, there has been a six-fold increase in overall exposure to medical sources of radiation.[20],[21] A recent estimate of all cancers attributable to medical radiation exposures in France found that the largest number was for breast cancer.[22]
- X-rays: Decades of research have confirmed the link between radiation and breast cancer in women who were irradiated for many different medical conditions, from tuberculosis[23] to benign breast disease[24],[25] and even acne.[26] Evidence from almost all conditions suggests that exposure to ionizing radiation during childhood and adolescence is particularly dangerous with respect to increased risk for breast cancer later in life,[27],[28],[29] and that there is a significant dose-response relationship between the dosage of childhood radiation and the increased incidence of breast cancer.[30]
- Computed tomography (CT) Scans: When a CT scan is directed at the chest, the individual receives radiation equivalent to 30 to 442 chest X-rays.[31] Other modeling suggests that 1 in 150 women who are 20 years old when they undergo CT angiograms of the chest, and 1 in 270 women of all ages having the procedure, will subsequently develop cancers of the chest, including breast cancer.[32]
- Mammography: Recent evidence indicates that the lower-energy X-rays provided by mammography resulted in substantially greater damage to DNA than would be predicted, and the effects of these exposures may be greatly underestimated when it comes to the risk of breast cancer.[33] For example, women who had multiple mammograms more than five years prior to diagnosis and started before age 35 had an increased risk of breast cancer.[34] Diagnostic radiation has been shown to increase risk for developing breast cancer in a dose-dependent manner for women who are BRCA positive and therefore more sensitive to radiation.[35]
- Radiation therapy: Researchers discovered a 16-fold increased relative risk of angiosarcoma (cancer of a blood vessel) in the breast and chest wall following irradiation of a primary breast cancer.[36] More recent data indicate that women younger than 45 who received the higher radiation exposure associated with post-lumpectomy radiotherapy had about a twofold increase in later contralateral breast cancer diagnoses. This effect was especially prominent in younger women with a significant family history of breast cancer.[37],[38],[39]
- Male breast cancer: Male breast cancer is relatively rare, but multiple exposures of men to medical radiation when they were young leads to a significant increase in risk for developing breast cancer several decades later.[40]
Backscatter security scanners
- Backscatter machines were put in place prior to a 2012 study that estimated that for every 2 million young girls who traveled by airplane once a week, one would develop breast cancer as a result.[41] In 2013, backscatter machines were removed from airports due to privacy concerns (not health concerns). Most airports now use millimeter wave screening, which does not use ionizing radiation.
Who is most likely to be affected by ionizing radiation?
Several factors interact with radiation to increase the potency of its carcinogenic effects:
- Age at exposure, genetic profile, and possibly estrogen levels.
- Direct exposure to radiation through military work or other occupations (listed above).
- Accidental or medical exposure to radiation more seriously affects children and adolescents than adults, with a greater chance of increasing their risk for breast cancer later in life.[42]
- CT angiography has been shown to cause a significant increase in risk of developing breast cancer, especially in pre-menopausal women.[43],[44]
- The effects of radiation on mammary carcinogenesis may be additive with effects of estrogens, as suggested by studies using human breast tumor cells in animals.[45],[46],[47] This is highly concerning due to the exposure levels of estrogen-mimicking chemicals in our environment.
Who is most vulnerable to the health effects of ionizing radiation?
- Everyone should be aware of the potential health hazards of ionizing radiation, but some women are more vulnerable than others to its health effects. Women carrying the BRCA1 mutation have deficits in many cell processes and a heightened sensitivity to the effects of radiation exposures.[48] These women are more likely to develop breast cancer and may be especially susceptible to the cancer-inducing effects of exposure to ionizing.[49],[50],[52],[51] This is especially true if women began exposures, including from mammography, at age 30 or earlier.[53]
- The detrimental risks from mammography might also be heightened in older women, whose breast epithelial cells have gone through several decades of cell division. Cells derived from older women’s breast tissue were more sensitive to the DNA-damaging effects of low-energy radiation, increasing the likelihood of later conversion to cancerous cells.[54]
- However, a recent laboratory study in rats indicates that having given birth and lactating the young was protective against development of breast cancers—especially ER+/PR+ tumors–in animals that had been exposed to radiation before puberty. This protective effect was not found if the animals had been exposed to the radiation as young adults.[55]
What are the top tips to avoid exposure?
- Discuss with your medical care team whether or not X-rays or CT scans are necessary and whether there are radiation-free alternatives. If you decide to seek out a second opinion, request that the original screening information be shared, to minimize the need for a second set of exposures if they are not necessary.
- Workers should follow recommended health and safety guidelines when working with any type of radiation, whether administering the radiation or taking part in a procedure where radiation is used.
- The U.S. Preventive Services Task Force recently recommended against the use of routine mammography screening before the age of 50 [56],[57] but supported the use of biennial screening between the ages of 50 and 75. Discuss with your doctor when you should begin regular mammograms, and how often they should be done, based on your individual family history and risk for breast cancer.
Updated 2019
[1] Brenner, David J et al. “Cancer risks attributable to low doses of ionizing radiation: assessing what we really know.” Proceedings of the National Academy of Sciences of the United States of America 100, 24 (2003): 13761-6. doi:10.1073/pnas.2235592100.
[2] United Kingdom National Radiation Protection Board. “Risk of radiation-induced cancer at low doses and low-dose rates for radiation protection purposes.” Documents of the NRPB 6, 25 (1995). https://www.researchgate.net/profile/Mark_Little/publication/254258458_Risk_of_radiation_induced_cancer_at_low_doses_and_low_dose_rates_for_radiation_protection_purposes/links/00b4952f3c62e5772f000000/Risk-of-radiation-induced-cancer-at-low-doses-and-low-dose-rates-for-radiation-protection-purposes.pdf.
[3] Goto, Hitomi et al. “Cancer mortality among atomic bomb survivors exposed as children.” Environmental Health and Preventive Medicine 17, 3 (2012): 228-34. doi:10.1007/s12199-011-0246-6.
[4] Pierce, D A et al. “Studies of the mortality of atomic bomb survivors. Report 12, Part I. Cancer: 1950-1990.” Radiation Research 146, 1 (1996): 1-27.
[5] Tokunaga, Masayoshi, et al. “Incidence of Female Breast Cancer among Atomic Bomb Survivors, 1950-1985.” Radiation Research 138, 2 (1994): 209–223. doi:10.2307/3578591.
[6] Land CE. “Studies of Cancer and Radiation Dose Among Atomic Bomb Survivors: The Example of Breast Cancer.” JAMA 1995;274(5):402–407. doi:10.1001/jama.1995.03530050050031.
[7] Brenner, Alina V et al. “Incidence of Breast Cancer in the Life Span Study of Atomic Bomb Survivors: 1958-2009.” Radiation Research 190, 4 (2018): 433-444. doi:10.1667/RR15015.1.
[8] Goldberg, Zelanna, and Bruce E Lehnert. “Radiation-induced effects in unirradiated cells: a review and implications in cancer.” International Journal of Oncology 21, 2 (2002): 337-49.
[9] Morgan, William F. “Non-targeted and delayed effects of exposure to ionizing radiation: II. Radiation-induced genomic instability and bystander effects in vivo, clastogenic factors and transgenerational effects.” Radiation Research 159, 5 (2003): 581-96. doi:10.1667/0033-7587(2003)159[0581:nadeoe]2.0.co;2.
[10] Tsai, Kelvin K C et al. “Cellular mechanisms for low-dose ionizing radiation-induced perturbation of the breast tissue microenvironment.” Cancer Research 65, 15 (2005): 6734-44. doi:10.1158/0008-5472.CAN-05-0703.
[11] Borrego-Soto, Gissela et al. “Ionizing radiation-induced DNA injury and damage detection in patients with breast cancer.” Genetics and Molecular Biology 38, 4 (2015): 420-32. doi:10.1590/S1415-475738420150019.
[12] Maier, Patrick et al. “Cellular Pathways in Response to Ionizing Radiation and Their Targetability for Tumor Radiosensitization.” International Journal of Molecular Sciences 17, 1 (2016): 102. doi:10.3390/ijms17010102.
[13] Brenner, Alina V et al. “Incidence of Breast Cancer in the Life Span Study of Atomic Bomb Survivors: 1958-2009.” Radiation Research 190, 4 (2018): 433-444. doi:10.1667/RR15015.1.
[14] Little, John B. “Genomic instability and radiation.” Journal of Radiological Protection 23, 2 (2003): 173-81. doi:10.1088/0952-4746/23/2/304.
[15] Harbron, Richard William. “Cancer risks from low dose exposure to ionising radiation – Is the linear no-threshold model still relevant?. ” Radiography 18, 1 (2012): 28-33. doi:101016/jradi201107003.
[16] Doody, Michele Morin et al. “Breast cancer incidence in U.S. radiologic technologists.” Cancer 106,12 (2006): 2707-15. doi:10.1002/cncr.21876.
[17] Simon, Steven L. et al. “Estimating Historical Radiation Doses to a Cohort of U.S. Radiologic Technologists.” Radiation Research 166, 1 (2006): 174–192. doi:10.1667/RR3433.1.
[18] Liu, Jason J. et al. “Work history and mortality risks in 90 268 US radiological technologists.” Occupational and Environmental Medicine 71, 12 (2014): 819-835. doi:10.1136/oemed-2013-101859.
[19] Ballard, T et al. “Cancer incidence and mortality among flight personnel: a meta-analysis.” Aviation, Space, and Environmental Medicine 71, 3 (2000): 216-24.
[20] Larson, David B et al. “National trends in CT use in the emergency department: 1995-2007.” Radiology 258, 1 (2011): 164-73. doi:10.1148/radiol.10100640.
[21] Linet, Martha S et al. “Cancer risks associated with external radiation from diagnostic imaging procedures.” CA: A Cancer Journal for Clinicians 62, 2 (2012): 75-100. doi:10.3322/caac.21132.
[22] Marant‐Micallef, Claire et al. “The risk of cancer attributable to diagnostic medical radiation: Estimation for France in 2015.” International Journal of Cancer 144: 2954-2963. doi:10.1002/ijc.32048.
[23] Mackenzie, I. “Breast Cancer Following Multiple Fluoroscopies.” British Journal of Cancer 19 (1965): 1–8. doi:10.1038/bjc.1965.1.
[24] Golubicic, I et al. “Risk factors for breast cancer: is ionizing radiation among them?.” Journal of B.U.ON.: Official Journal of the Balkan Union of Oncology 13, 4 (2008): 487-94.
[25] Mattsson, A. et al. “Dose- and time-response for breast cancer risk after radiation therapy for benign breast disease.” British Journal of Cancer 72 (1995): 1054–1061. doi:10.1038/bjc.1995.461.
[26] El-Gamal, Hazem and Richard G Bennett. “Increased breast cancer risk after radiotherapy for acne among women with skin cancer.” Journal of the American Academy of Dermatology 55, 6 (2006): 981-9. doi:10.1016/j.jaad.2005.10.005.
[27] John, Esther M et al. “Medical radiation exposure and breast cancer risk: findings from the Breast Cancer Family Registry.” International Journal of Cancer 121, 2 (2007): 386-94. doi:10.1002/ijc.22668.
[28] Koo, Eva et al. “Management and Prevention of Breast Cancer After Radiation to the Chest for Childhood, Adolescent, and Young Adulthood Malignancy.” Annals of Surgical Oncology 22, 3 (2015): S545-51. doi:10.1245/s10434-015-4596-y.
[29] Pijpe, Anouk et al. “Exposure to diagnostic radiation and risk of breast cancer among carriers of BRCA1/2 mutations: retrospective cohort study (GENE-RAD-RISK).” BMJ (Clinical Research Edition) 345 (2012): e5660. doi:10.1136/bmj.e5660.
[30] Inskip, Peter D et al. “Radiation-Related New Primary Solid Cancers in the Childhood Cancer Survivor Study: Comparative Radiation Dose Response and Modification of Treatment Effects.” International Journal of Radiation Oncology, Biology, Physics 94, 4 (2016): 800-7. doi:10.1016/j.ijrobp.2015.11.046.
[31] Redberg, Rita F. “Cancer risks and radiation exposure from computed tomographic scans: how can we be sure that the benefits outweigh the risks?.” Archives of Internal Medicine 169, 22 (2009): 2049-50. doi:10.1001/archinternmed.2009.453.
[32] Smith-Bindman, Rebecca et al. “Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer.” Archives of Internal Medicine 169, 22 (2009): 2078-86. doi:10.1001/archinternmed.2009.427.
[33] Heyes, G J, A J Mill and M W Charles. “Mammography-oncogenecity at low doses.” Journal of Radiological Protection 29, 2A (2009): A123-32. doi:10.1088/0952-4746/29/2A/S08.
[34] Ma, Huiyan et al. “Low-dose medical radiation exposure and breast cancer risk in women under age 50 years overall and by estrogen and progesterone receptor status: results from a case-control and a case-case comparison.” Breast Cancer Research and Treatment 109, 1 (2008): 77-90. doi:10.1007/s10549-007-9625-5.
[35] Pijpe, Anouk et al. “Exposure to diagnostic radiation and risk of breast cancer among carriers of BRCA1/2 mutations: retrospective cohort study (GENE-RAD-RISK).” BMJ (Clinical Research Edition) 345 (2012): e5660. doi:10.1136/bmj.e5660.
[36] Huang, Jenny and Willian J. Mackillop. “Increased risk of soft tissue sarcoma after radiotherapy in women with breast carcinoma.” Cancer 92 (2001): 172-180. doi:10.1002/1097-0142(20010701)92:1<172::AID-CNCR1306>3.0.CO;2-K.
[37] Hooning, Maartje J. et al. “Roles of Radiotherapy and Chemotherapy in the Development of Contralateral Breast Cancer.” Journal of Clinical Oncology 26, 34 (2008): 5561-5568. doi:10.1200/JCO.2007.16.0192.
[38] Ng, Andrea K, and Lois B Travis. “Radiation therapy and breast cancer risk.” Journal of the National Comprehensive Cancer Network 7,10 (2009): 1121-8. doi:10.6004/jnccn.2009.0073.
[39] Stovall, Marilyn et al. “Dose to the contralateral breast from radiotherapy and risk of second primary breast cancer in the WECARE study.” International Journal of Radiation Oncology, Biology, Physics 72, 4 (2008): 1021-30. doi:10.1016/j.ijrobp.2008.02.040.
[40] Abdelwahab Yousef, Ali Jad. “Male Breast Cancer: Epidemiology and Risk Factors.” Seminars in Oncology 44, 4 (2017): 267-272. doi:10.1053/j.seminoncol.2017.11.002.
[41] Mehta, Pratik, and Rebecca Smith-Bindman. “Airport full-body screening: what is the risk?.” Archives of Internal medicine vol. 171,12 (2011): 1112-5. doi:10.1001/archinternmed.2011.105.
[42] Boice, John D. Jr. “Radiation and breast carcinogenesis.* Medical and Pediatric Oncology 36: 508-513. doi:10.1002/mpo.1122.
[43] Huda, Walter et al. “Radiation-related cancer risks in a clinical patient population undergoing cardiac CT.” American Journal of Roentgenology 196, 2 (2011): W159-65. doi:10.2214/AJR.10.4981.
[44] Einstein, Andrew J et al. “Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography.” JAMA 298, 3 (2007): 317-23. doi:10.1001/jama.298.3.317.
[45] Calaf, Gloria M. and Tom K. Hei. “Establishment of a radiation- and estrogen-induced breast cancer model.” Carcinogenesis 21, 4 (2000): 769–776. https://doi.org/10.1093/carcin/21.4.769.
[46] Imaoka, Tatsuhiko et al. “Radiation-induced mammary carcinogenesis in rodent models: what’s different from chemical carcinogenesis?” Journal of Radiation Research 50, 4 (2009): 281-93. doi:10.1269/jrr.09027.
[47] Segaloff, Albert and William S. Maxfield. “The synergism between radiation and estrogen in the production of mammary cancer in the rat.” Cancer Research 31 (1971): 166–168.
[48] Baert, Annelot et al. “Increased chromosomal radiosensitivity in asymptomatic carriers of a heterozygous BRCA1 mutation.” Breast Cancer Research 18, 1 (2016): 52. doi:10.1186/s13058-016-0709-1.
[49] Andrieu, Nadine et al. “Effect of chest X-rays on the risk of breast cancer among BRCA1/2 mutation carriers in the international BRCA1/2 carrier cohort study: a report from the EMBRACE, GENEPSO, GEO-HEBON, and IBCCS Collaborators’ Group.” Journal of Clinical Oncology 24, 21 (2006): 3361-6. doi:10.1200/JCO.2005.03.3126.
[50] Berrington de Gonzalez, Amy et al. “Estimated risk of radiation-induced breast cancer from mammographic screening for young BRCA mutation carriers.” Journal of the National Cancer Institute 101, 3 (2009): 205-9. doi:10.1093/jnci/djn440.
[51] Pepe, Stefano, Matilde Pensabene and Caterina Condello. “Modifiers of Risk in BRCA1/2 Mutation Carriers.” Current Women`s Health Reviews 8, 1 (2012): 23-29. doi:10.2174/157340412799079246.
[52] Turnbull C, N Mirugaesu and R Eeles. “Radiotherapy and genetic predisposition to breast cancer.” Clinical Oncology 18, 3 (2006): 257-267. doi:10.1016/j.clon.2005.11.013.
[53] Colin, Catherine et al. “Radiation induced breast cancer risk in BRCA mutation carriers from low-dose radiological exposures: A systematic review.” Radioprotection. 52, 4 (2017): 231–40. doi:10.1051/radiopro/2017034.
[54] Soler, David et al. “Radiation sensitivity increases with proliferation-associated telomere dysfunction in nontransformed human epithelial cells.” Aging Cell 8, 4 (2009): 414-25. doi:10.1111/j.1474-9726.2009.00488.x.
[55] VoPham, Trang et al. “Environmental radon exposure and breast cancer risk in the Nurses’ Health Study II.” Environmental Health 16, 1 (2017): 97. doi:10.1186/s12940-017-0305-6.
[56] Nelson, Heidi D et al. “Screening for breast cancer: an update for the U.S. Preventive Services Task Force.” Annals of Internal Medicine 151, 10 (2009): 727-37. doi:10.7326/0003-4819-151-10-200911170-00009.
[57] US Preventive Services Task Force. “Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement.” Annals of Internal Medicine 151, 10 (2009): 716-26. doi:10.7326/0003-4819-151-10-200911170-00008.
Types: Article